What Treatment Options Are Available for Cystoceles?
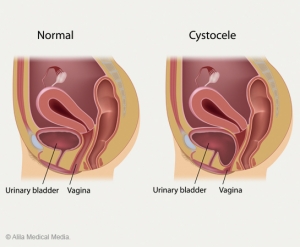 An Overview of a Prolapsed Bladder & Cystocele Repair Surgery
An Overview of a Prolapsed Bladder & Cystocele Repair Surgery
What are Uterine Fibroids?
“I Have Uterine Fibroids. Should I be concerned?”
The doctors that make up Women’s Specialists of Plano see their fair share […]
2010 Medical Mission to Guatemala
Dr. Murray Fox, a Plano gynecologist, and Dr. Daryl Greebon, a Plano OBGYN, of Women’s Specialists of Plano […]
Robot-Assisted Hysterectomy
Robot-Assisted Hysterectomy an Innovative Treatment Option
The physicians at Women’s Specialists of Plano are among the more experienced gynecologic robotic surgeons […]
Endometrial Ablation as a Menorrhagia Treatment
 Dr. Jules Monier performs endometrial ablation […]
Dr. Jules Monier performs endometrial ablation […]
What Are the Solutions For Urinary Incontinence?
Facts About Urinary Incontinence and Uterine Prolapse Treatment
What Do I Need to Know About Urinary Incontinence?
Facts About Urinary Stress Incontinence And Uterine Prolapse
Author: Dr Daryl Greebon with Women’s Specialists of Plano
There […]
Can You Explain More About Uterine Fibroids?
An Overview of Uterine Fibroids
Many women living in the communities of Plano, Frisco and Dallas, Texas experience non-cancerous tumors in […]


